مركز ابحاث وتطوير المثلث
جمعية أالزهراوي
Triangle Research & Development Center
Years of Igniting Innovation
Advancing Applicable Research, Technological Development, And Community Empowerment
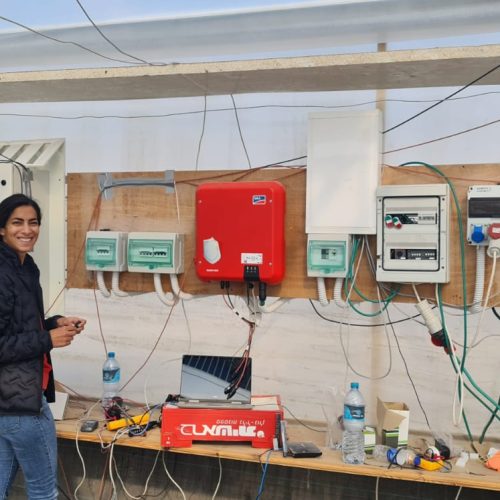
Applicable Research
We operate in a broad range of fields from AgriVoltaics, Biochemistry, Computer Science, Biology, Physics, Social Sciences, and more.
Technological Development
We strive to bridge the gap between applicable R&D and innovative commercial development, fostering invention excellence.
Community Involvement
Our dedication is to improve the quality of science education in the Triangle region throughout the Science Gardens' innovative projects
InnoWadi Group Incubator
The place to identify, nurture and transform the TRDC inventions into products
InnoWadi Group controls TRDC’s intellectual assets and provides corporate frameworks to develop and advance scientific applications via subsidiaries, strategic partnerships, concessions and licensing agreements. InnoWadi facilitates intellectual property rights management and technology transfer while providing support for collaboration and mediate relationships between different innovation stakeholders, such as academia and industry.
Scientific Applicable Research
Dive into the TRDC scientific Breakthroughs
The Triangle R&D Center is devoted to serve the community through promoting and developing scientific applicable research, by finding solutions that serve and support our societies in different fields, such as AgriVoltaics, Agriculture, Heritage studies, Health, Biology, Chemistry, HDIA, and environmental researches funded by winning competitive research grants in Israel and abroad.
The center further advances community research related to issues of education and addressing gender inequalities, with a goal to promote the role of women in science and leadership.
...
With And For The Community























Al-Zahrawi Association Founder, M.D. , Uricont Founder, History of Science

Computer Science, HDIA, Machine Learning; Pattern Recognition;; Neural Networks..

PhD Candidate at Tel Aviv University

Semi-Transparent Flexible Photovoltaic Films

Public Health and Environmental
Medical Microbiology and the Epidemiology of Nosocomial Infections
Neurodevelopmental Disorders

Medical and Agricultural applications of Molecular Encapsulation of Active Ingredients
Political Science and Sociology

Machine Learning, Document Image Analysis DIA

Nano-Photonics Research Fellow at Tel Aviv University
Biochemistry, Biophysics and Molecular Biology
PARTNERS

























Dr. Ibrahim Yehia
TriSolar Founder, Triangle R&D Center Chief Officer - Solar Energy Group Researcher